Sprained Ankle
Tissues commonly affected
Keywords; sprained ankle, chiropractic help.
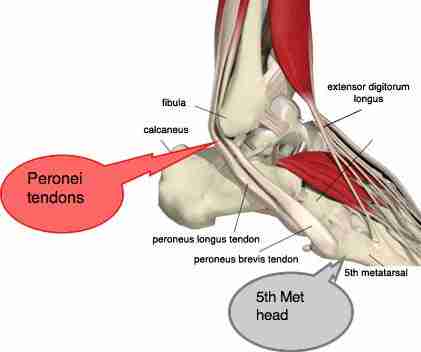
Lower leg injuries often occur when there is weakness of one or more muscles on the side of the lower leg, commonly one of the Peroneus muscles. Normally these muscles should prevents the ankle from twisting, most commonly inwards, called inversion.
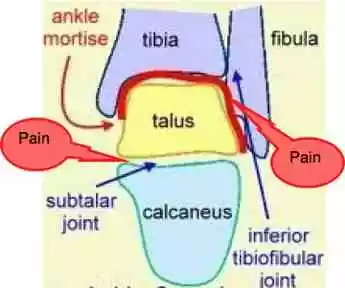
The talus bone moves mainly in one mode, called dorsi and plantar flexion; up and down. When an ankle is sprained, the bone subluxates within its socket, see below, causing jamming. This is what causes the severe, sharp pain of a sprain.
The talus may remain partly locked for years, if not correctly freed with the appropriate adjustment, changing the whole movement pattern of the foot, knee and hip. At chiropractic coalface 2 you can read about how the Dutch national marathon champion had to stop running because of knee pain that was directly caused by an untreated ankle sprain.
The talus sits on top of the calcaneus, or heel bone, in what is known as the subtalar joint. Can you also see the ankle mortice in the pictures below?
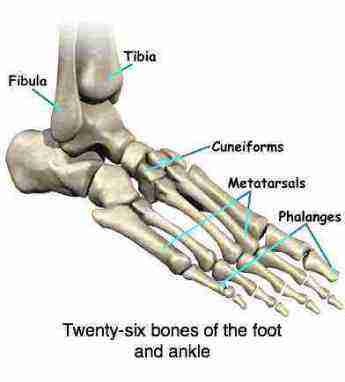
There are so many bones and joints, with so much pain potential.
The joint or, ankle mortise, as it is called, is formed between two leg bones, the tibia and the fibula and the talus.
The talus fits snugly into a socket formed by the tibia and the fibula, moving like a hinge and allowing the foot to move up and down, supported by an array of ligaments.
Trauma is probably the most common cause of ankle joint pain, but other conditions like a flat foot, or an arthritic hip that change the gait could also be a factor.
Very serious injuries can happen to this complex as you can read about in this ankle joint pain casefile.
The more common fractures are of the ends of the long bones, the tibia and fibula. However, fracture can occur of any of the ankle bones.
Whenever there's enough force to break a bone, assume that there have been torn ligaments too.
How reliable are xrays? A missed fracture can have terrible consequences for the ankle. Scroll down for this case of avascular necrosis.
Careful correction of any ankle mortise and subtalar joint subuxations is a very important, and oft neglected, part of the successful treatment of a sprained ankle.
Ankle mortise and Subtalar joints
LIGAMENTS
There are ligaments on both sides of the ankle that hold the bones together. They give the joint stability. They connect bones together while tendons connect muscles to the osseous structures.
In an inversion sprained ankle, the most common injury, usually it is the ligaments on the outer side that are stretched and occasionally ruptured. Bruising is a sign that there has been some tearing of the tissues.
Should that correction of the subluxations in the ankle not be done, it leads to vital changes to the biomechanics of the foot. This is usually the underlying cause of chronic pain, plantar myofascitis and more difficult to predict changes in the knees, hips and spine.
Yes, that arthritic knee may be the result of an old ankle injury that wasn't properly cared for.
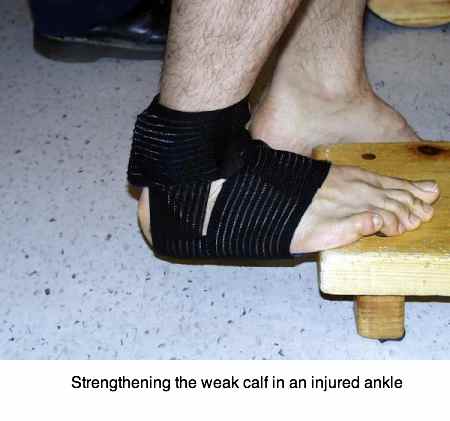
An ankle guard may be useful during the healing phase of the damaged ligaments. Research shows that small movements of the joint, rather than total immobilization as in a cast, for example, promotes faster healing in the treatment of a sprained lower limb.
The trend today is towards a boot that limits movement, provides pressure to reduce swelling, but can be removed for icing, bathing and gentle non weight bearing exercises.
Crutches may be vital for a period in a serious injury. However, keep the ankle mobile and moving, gently if it's swollen and sore, by doing the alphabet exercises. Soon something coming up on YouTube for you, but for the moment just wriggle the joint about whilst you are sitting.
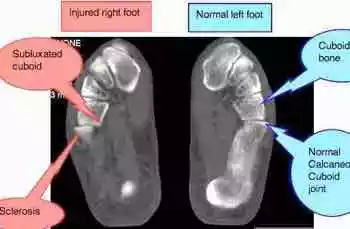
A strong recommendation; if you know your ankle is not getting better, get a scan. Fractures of the one of the tarsal bones lurk and are often missed on plain xrays, sometimes with very serious consequences.
Muscles of the ankle
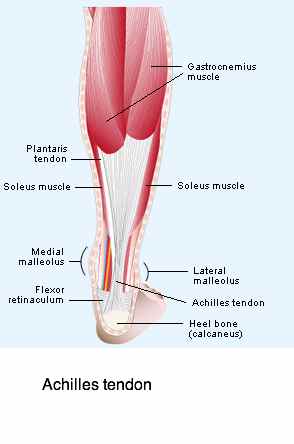
There are also many tendons that cross the ankle to move the foot and the toes. Tendons connect muscle to bone, enabling you to move your foot.
The muscles usually affected lie on the outer side of the lower leg. There are three of them called the peronei group, plus a few others, mainly for moving the toes.
The contraction of Peroneus Brevis may be so sudden and severe, in attempting to prevent inversion ankle sprain, that it ruptures off its attachment to the bone. This is called a Jones fracture and immobilisation in a cast is essential.
Sprained Ankle Treatment @ Chiropractic Help
- Displaced bones are often associated with sprained ankle, usually the Talus bone, the Calcaneus bone and the Cuboid bone. Correction of these subluxations is an essential part of the treatment of a sprained ankle. For more about the immobilisation arthritis that comes from uncorrected subluxations.
- The ankle ligaments may be associated with ankle sprain, with stretching and possible tearing of these ligaments. Swelling and bruising are common findings. Rupture is uncommon.
- Muscle and tendon sprain may also occur. The achilles tendon and the muscle on the outer part of the leg are most frequently involved in ankle sprain.
- Less commonly, bones may be fractured in a sprained ankle. Most usually the knobby on the outer side of the ankle (the lateral maleolus) and the end of a bone on the side of the foot may be involved. They are the attachments for the ligaments and tendons of the ankle which are often stronger than the bone itself (aka an avulsion fracture ). Immobilisation is then essential, and occasionally a pin or plate may be necessary if a fracture has occurred in your ankle sprain. It doesn't take much imagination to guess this is a job for a good orthopaedic surgeon ...
There is some interesting research that magnetic care may help in the healing of ankle fractures and sprained ankle.
ANKLE SPRAIN TREATMENT
- ICE should immediately be applied after a sprain of the ankle. This can best be done with an ice block immediately over the effected painful area.
- COMPRESSION may be important if it starts to swell. This is done with a compression bandage which should be professionally applied, but needs to be loosened regularly to allow movement of the joint (which has been shown to promote healing) and so that ice can be applied.
- ELEVATION is necessary if more extreme swelling occurs. X-RAY may be important to rule out fracture. It will then need to be cast for 6 weeks. A crack may not show up immediately, so the X-ray may need to be repeated after 10 days if fracture is still suspected.
- CHIROPRACTIC HELP management of this very painful condition is particularly successful because it addresses subluxation of bones that usually occurs, and looks for the underlying cause which may be in the low back or sacro-iliac joint. Remember, it is the weakness of a muscle that allows the ankle to invert and sprain.
- REHABILITATION of the ankle is essential. For more aboutankle exercises ,
LIGAMENTS
Gentle stretching of sprained ligaments is important. The alphabet ankle exercises are equally effective for your ligaments.
"If it's not fun, it's not worth doing. And it doesn't have to be silly. It can be hard work and it can be edgy. It can be a lot of things. But it can also be fun."
Robert Redford
Muscles
An ankle sprain often strains muscles and their tendons. Most particularly the muscles on the side of your lower leg (called the Peronei; there are three, Longus, Brevis and Tertius) together with the gastrocnemius and its Achilles tendon.
To exercise the Peronei, lie on the floor and hook your kapot bicycle tube over your foot, and the other end over some fixed point on the other side of your foot. Start by pulling the toes towards your head against the pull of the tube, then do it an an angle. They are difficult muscles to stretch without putting undue stress on the injured joints.
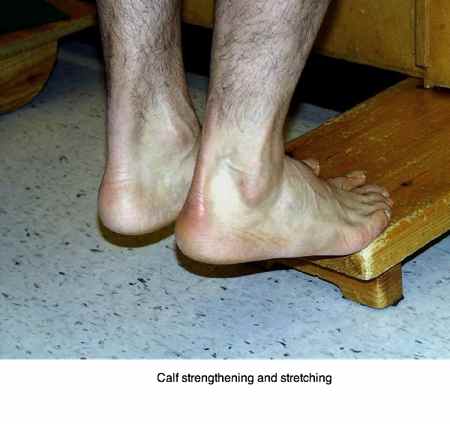
To exercise the Gastrocnemius mucles (and its oft forgotten companion, the Soleus, the cause of Shin Splints stand on a hard floor, go up on your toes. Start using both feet together, gradually putting more weight on the injured foot. Do this regularly through the day.
To make it more difficult, stand on the balls of your feet on a step. Go up on your toes, and then sink deep, before flexing your ankle again. Do it with the ankle guard on to begin.
These are simple and effective ankle exercises, things you can do for yourself. They cost nothing, just a little time and discipline! Otherwise you will be visiting your chiropractor endlessly! Saving you time, saving you money ...
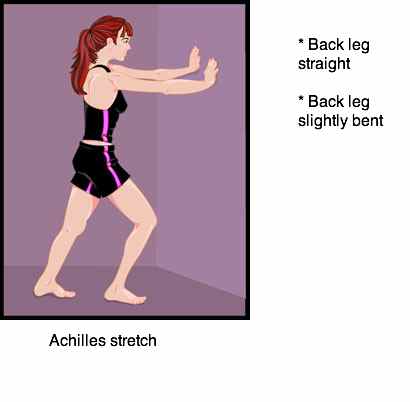
To stretch the Achilles, stand with your injured leg about a metre from a wall. Put the other foot forwards. Reaching forwards, keeping your heel on the ground, stretch the achilles,
- first with the knee straight, and
- then slightly bent.
You won't be able to do this if the talus is still fixated - you will get sharp pain, deep within the ankle. First have the joint adjusted.
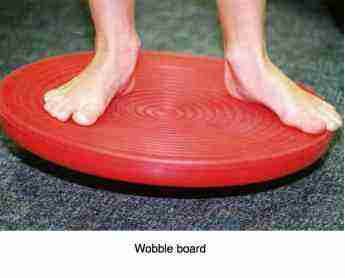
Buy yourself a wobble board to do proprioception training after an ankle injury. Start with sports shoes to give the ankle support, but graduate as soon as possible to bare feet when doing your ankle exercises.
Walking
Walking is of course the best of your outdoor ankle exercises. Normally we would suggest that you don't walk on tarmac or concrete, but in this instance it is recommended. That ankle can turn again VERY easily if the ankle ligaments have been torn. So do it on a level surface, with your ankle support and good shoes.