Lateral Femoral Cutaneous Nerve Entrapments
By Scott Cuthbert, DC
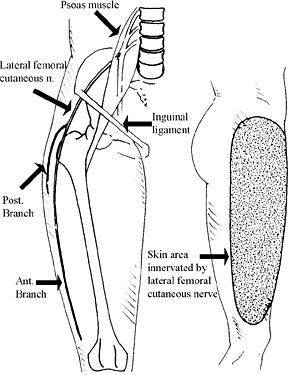
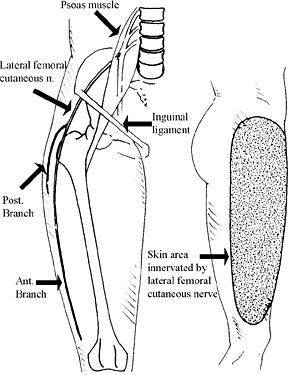
The lateral femoral cutaneous nerve arises from the 2nd and 3rd lumbar nerves. It is formed in the psoas muscle1 and emerges from its lateral border to cross the iliacus muscle and exit the pelvis.
The most common point for possible entrapment is as the nerve passes between the two slips of the inguinal ligament's lateral attachment to the anterior-superior iliac spine, where it exits the pelvis. The nerve is tightly bordered by the tendinous fibers of the inguinal ligament at this point and makes a right-handed bend to change direction from a horizontal course in the pelvis to a more vertical course in the lateral and anterolateral thigh. The lower slip of the inguinal ligament also gives origin to some sartorius fibers.2 The nerve may pass in front of or through the sartorius into the thigh.3
Shortly after it leaves the abdomen, the nerve divides into an anterior and a posterior branch. The anterior branch supplies the skin of the anterior and lateral parts of the thigh to the knee. The posterior branch supplies the skin on the lateral surface of the thigh, from the greater trochanter down the lateral thigh. The lateral femoral cutaneous nerve is strictly sensory, giving no motor supply.
As the nerve reaches a point just medial to the anterior-superior iliac spine where it enters the thigh, it changes its course from nearly horizontal to vertical. This angulation is increased by extension and lessened by flexion of the thigh. In addition to this major point of possible entrapment, other locations may be where the nerve emerges from the psoas muscle,
4 the passage underneath the
fascia lata, and the area where the nerve leaves the fascia.
2
After the lateral femoral cutaneous nerve exits the pelvis at the opening of the inguinal ligament, it is held down as it pierces the fascia lata; thus, movement between the thigh and pelvis can stretch the nerve and increase entrapment at the opening of the inguinal ligament.
5
Entrapment is prone to occur in obesity, with a lax abdominal wall, and in pregnancy.2, 6Diabetics have an increased susceptibility to compression neuropathy, which is especially apparent in this nerve.7
Symptoms of Nerve Entrapment
Nerve entrapment causes pain called
meralgia paresthetica (Barnhardt-Roth syndrome) in the anterolateral thigh.6,8 ( Interestingly, Sigmund Freud reported in 1895 that he and one of his sons suffered from the condition.)
9 The condition affects men more than women due to possible occupational considerations, and can also be bilateral in some 25 percent of cases.
10 It most commonly develops from the nerve's fascial attachment in the thigh pulling the nerve tightly against the opening at the lateral end of the inguinal ligament,
2 which usually relates to thigh obesity and/or a lateral shift in trunk posture.
4 Generally, meralgia paresthetica develops without prior trauma.
Other symptoms consist of increased 2 or decreased sensitivity. 6 Rubbing of clothing and other cutaneous stimuli causes a characteristic burning pain on the outer side of the thigh. Pelvic and hip motion, such as walking and running, aggravates the pain. In general, those with meralgia paresthetica have poor posture; consequently, the postural muscles are overactive and fatigued with prolonged standing, which also aggravates pain.
The postural deficiency most common with meralgia paresthetica is lumbar hyperlordosis and a protuberant abdomen.
4,11 Manual muscle testing examination usually finds weak abdominal and gluteus maximus muscles failing to provide support to prevent anterior rotation of the pelvis, with subsequent hyperlumbar lordosis.
11 Aggravating the condition will probably be hypertonic lumbar extensor muscles and shortening of
the iliopsoas. Sitting and recumbent positions relieve the pain; however, sitting with one leg crossed over the other – especially the ankle on the knee – can exacerbate the pain.
Postural shifts by a short leg, whether physiological or anatomical, may be a factor in the condition. Other factors include the muscle fibers from the internal oblique and transverses abdominus muscles originating from the inguinal ligament, or the external oblique muscle inserting into it.3 Additional causes have been reported, including body-building,12 falling asleep in Siddha yoga position,13 seat-belt14 and pocket-watch trauma,15 and misplaced injections.16
Presentation and Diagnosis
Meralgia paresthetica presents more often to chiropractors than is generally recognized.17 In 215 consecutive examinations of patients in a chiropractic office, 12 cases of meralgia paresthetica were diagnosed. The method of diagnosis was "standard orthopedic and neurologic testing procedures that evaluate the lateral femoral cutaneous nerve territory for superficial tactile sensation, superficial pain, sensitivity to vibration, sensitivity to temperature, and temperature gradient studies."18
Patients had been aware of their condition from two days to 12 years. Five of the 12 had received treatment by the medical profession, with an unsatisfactory diagnosis or results.
The condition should be differentially diagnosed from conditions such as 2nd and 3rd lumbar nerve root compression, appendicitis, spinal cord tumor, colon cancer, and trochanteric or iliopsoas bursitis.2 Disturbance at the lumbar level is usually associated with diminished or absent patellar reflex and weakness of the quadriceps muscles. Because the lateral femoral cutaneous nerve is purely sensory, there is never weakness or reflex change when disturbance is limited to its entrapment.2, 6
In femoral neuropathy or L2-3 root lesions, sensory changes usually spread out to extend more anteromedially than in entrapments of the lateral femoral cutaneous nerve, where the sensory change is limited to its dermatome.
6 Staal
19 considers meralgia paresthetica rare and suggests that "one should look carefully for vertebral or
disc lesions, intrapelvic anomalies, old operation scars, compression from outside due to clothing or chronic microtrauma: in short for all kinds of local pathology along the course of the nerve, from its beginning until distal to the anterior superior iliac spine. In the majority of the cases no obvious cause will however be found even after thorough investigation."
Failure to find a cause for meralgia paresthetica is not consistent with chiropractic findings. This may be due to a more functional evaluation of spinal, pelvic and muscular function with chiropractic methods.
There will usually be pain below and slightly medial to the anterior superior iliac spine, close to the inguinal ligament attachment. To determine the attachment of the inguinal ligament, palpate along the ligament to the bone. A positive indication that meralgia paresthetica is present occurs when deep pressure in this area causes radiation of pain in the skin supplied by the lateral femoral cutaneous nerve.
Another source of pain at the anterior superior iliac spine is the origin of the sartorius, especially when there is a category II pelvic involvement. Since skeletal muscular imbalance is often present in meralgia paresthetica, sartorius pain and a category II may be present in combination with lateral femoral cutaneous nerve entrapment. To differentiate sartorius pain, palpate its origin at the anterior superior iliac spine and the upper half of the notch below it. From the sartorius origin, palpate down the sartorius tendon into the muscle, observing for pain; this indicates muscle involvement rather than, or in addition to, nerve entrapment. Usually the muscle will also test weak.
Low back derangement may cause pain in the greater trochanteric region or in the tensor fascia lata. It is distinguished from meralgia paresthetica by the absence of sensory alteration in the skin, and lack of pain on digital pressure to the nerve.4
Entrapment of the superior gluteal nerve that supplies the gluteus medius and minimus and tensor fascia lata, as well as the greater trochanteric region and a portion of the hip joint, can cause what has been termed false meralgia paresthetica.2 In this condition there is pain over the gluteus medius and minimus that radiates down the lateral aspect of the thigh to the knee. Lack of cutaneous sensory findings and no tenderness of the lateral femoral cutaneous nerve differentiate this from true meralgia paresthetica. Structural correction of the spine and pelvis typically corrects the condition.
Body language that first indicates that entrapment of the lateral femoral cutaneous nerve and meralgia paresthetica may be present is the location of the pain, and whether it is relieved in seated or recumbent positions and exacerbated by standing, walking and hip extension. Hip extension applied as a provocative test for meralgia paresthetica will aggravate the paresthesia and discomfort.20
A therapeutic test that is sometimes done is a local anesthetic injection at the point of probable entrapment.21 Williams and Trzil21 reported on an impressive series of 277 patients for whom only 24 cases required surgery. In a surgical study for the relief of meralgia paresthetica, there were findings of constrictive fascial bands around the lateral femoral cutaneous nerve in 19 of 21 cases, indicating that soft-tissue disturbances of the mechanical interface with the nerve the most common etiology.22
Corrective Strategies
Correction of entrapment of the lateral femoral cutaneous nerve is usually readily accomplished using chiropractic techniques. Even without the effective procedures of applied kinesiology, exercises directed toward improvement of muscles that support the pelvis – especially the abdominals – have been shown to be effective in treating this condition.4 Surgical procedures are usually not done as a method of treatment.23 Correction of spinal subluxations has been indicated as a method of treatment.4 Obviously, the optimal approach is to evaluate all aspects of the condition and correct any dysfunction that is present.

There is usually a pelvic category I or II and weak abdominal and gluteus maximus muscles. Total
postural balance should be evaluated and corrected, as well as modular interaction of PRYT, cloacal synchronization, and dural tension.11, 24 These techniques restore organization to the muscles and postural balance, and are often important in improving range of motion.
A painful myofascial trigger point (MTrP) may be found just medial to the anterior superior iliac spine.25 Muscle stretch reaction of the hip flexors differentiates this from radiating pain due to pressure on the entrapped nerve. The trigger point is treated with the usual chiropractic methods of percussion, trigger-point pressure release, or stretch-and-spray methods.11,24,26
A recently published systematic review of the literature on the chiropractic management of myofascial trigger points and myofascial pain syndromes27 reviewed 112 publications and came to the recommendation that moderately strong evidence supports some manual therapies (manipulation and ischemic pressure) for immediate pain relief for myofascial trigger points.
After these chiropractic techniques have been applied, evaluate hip extension range of motion; if limited, evaluate the hip flexors for muscle stretch reaction and apply either trigger point pressure release, percussion, or stretch and spray technique to obtain improved range of motion. Frequently the percussion and/or trigger point pressure release technique is the appropriate one. This appears to release the fascial pull on the lateral femoral cutaneous nerve that is causing the entrapment at its pelvic outlet. Stretching exercises designed to stretch the iliopsoas and rectus femoris muscles are usually contraindicated since they will cause additional irritation to the entrapped nerve. Generalized body organization or local muscle treatment is usually satisfactory for obtaining effective correction.
Medical approaches have included ultrasound at L2 and where the nerve leaves the pelvis; and high-voltage electrogalvanic stimulation. "The medical approach, after attempting to relieve external stress to the nerve, would include mild analgesia or local injection of xylocaine or corticosteroids."28 These procedures are usually not necessary in a comprehensive chiropractic practice.
Kopell and Thompson
29 found that
stretching exercises to relax the tensor fascia lata and shoe lifts are ineffective. They do, however, state that most often the condition can be corrected without neurolysis.
References
- Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy, 6th Edition. Lippincott Williams & Wilkins; 2009.
- Staal A, van Gijn J, Spaans F. Mononeuropathies: Examination, Diagnosis and Treatment.WB Saunders: London; 1999.
- Gray's Anatomy: The Anatomical Basis of Clinical Practice. Churchill Livingstone: Edinburgh; 2004.
- Skaggs CD, Winchester BA, Vianin M, Prather H. A manual therapy and exercise approach to meralgia paresthetica in pregnancy: a case report. J Chiropr Med, 2006;5(3):92-6.
- Kopell HP, Thompson WAL. Peripheral Entrapment Neuropathies, 2nd Edition. Robert E. Krieger Pub Co: Huntington, NY; 1976.
- Harney D, Patijn J. Meralgia paresthetica: diagnosis and management strategies. Pain Med, 2007;8(8):669-77.
- Veves A, Giurini JM, LoGerfo FW. The Diabetic Foot: Medical and Surgical Management.Humana Press: Totowa, NJ; 2002.
- Pearce JM. Meralgia paraesthetica (Bernhardt-Roth syndrome). J Neurol Neurosurg Psychiatry, 2006;77(1):84.
- Freud S. Ueber die Bernhardtsche Sensibilitaetsstoreung. Neurol Centralbl, 1895. 14491–14492.
- Sunderland S. Nerves and Nerve Injuries, 2nd Edition. Churchill-Livingstone: New York; 1978.
- Cuthbert S. Applied Kinesiology: Clinical Techniques for Lower Body Dysfunctions. The Gangasas Press: Pueblo, CO; 2013.
- Szewczyk J, Hoffmann M, Kabelis J. Meralgia paraesthetica in a body-builder. Sportverletz Sportschaden, 1994;8(1):43-5.
- Mattio TG, Nishida T, Minieka MM. Lotus neuropathy: report of a case. Neurology,1992;42(8):1636.
- Beresford HR. Meralgia paresthetica after seat-belt trauma. J Trauma, 1971;11(7):629-30.
- Mack GJ. Watchpocket meralgia paresthetica. IMS Ind Med Surg, 1968;37(10):778-9.
- Ecker AD, Woltman HW. Meralgia paresthetica: a report of one hundred and fifty cases. 1938;110:1650-1652.
- Arcadi VC. Lower back pain in pregnancy: chiropractic treatment and results of 50 cases.Collected Papers International College of Applied Kinesiology, Shawnee Mission, KS. 1996: 55-57.
- Kadel RE, Godbey WD, Davis BP. Conservative and chiropractic treatment of meralgia paresthetica: Review and case report. J Manip Physiol Ther, 1982;5(2):73-8.
- Staal A. The Entrapment Neuropathies. In: Handbook of Clinical Neurology, Volume 7. (Editors: Vinken PJ, Bruyn GW). American Elsevier Pub Co.: New York; 1970.
- Russell SM. Examination of Peripheral Nerve Injuries: An Anatomical Approach. Thieme Medical Publishers, Inc.: New York; 2006.
- Williams PH, Trzil KP. Management of meralgia paresthetica. J Neurosurg, 1991;74(1):76-80.
- Edelson R, Stevens P. Meralgia paresthetica in children. J Bone Joint Surg (U.S.), 1994;76(7):993-9.
- Aguayo AJ. Neuropathy Due to Compression and Entrapment. In: Peripheral Neuropathy, Vol I. (Editors: Dyck PJ,. Thomas PK, Lambert EH). W.B. Saunders Co: Philadelphia; 1975.
- Walther DS. Applied Kinesiology Synopsis, 2nd Edition. ICAKUSA: Shawnee Mission, KS; 2000.
- Biemond A. Femoral Neuropathy. In: Handbook of Clinical Neurology, Volume 8. (Editors: Vinken PJ, Bruyn GW). American Elsevier Pub Co: New York; 1970.
- Cuthbert S. Applied Kinesiology and the Myofascia. Int J AK and Kinesio Med, 2002;13-14.
- Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: a systematic review of the literature. J Manipulative Physiol Ther, 2009;32(1):14-24.
- Stites JS. Meralgia paresthetica: a case report. Research Forum, 1986;2(2).
- Kopell HP, Thompson WAL. Peripheral entrapment neuropathies of the lower extremity. N Engl J Med, 1960;262:56-60.