Head Neck pain
What's needed is a classification system to determine just how bad our head neck pain is.
It still astonishes me how often I have a new patient with a cervical spine problem of several decades duration who has never consulted a chiropractor. Fifty years ago I can understand; there weren't too many DCs around in those days.
But to have been suffering all those years, gulping down prodigious quantities of pills that are known to poison the kidneys, or just suffering in misery, makes absolutely no sense when science proves so conclusively what causes migraine, for example.
Here's a quote from the Kidney Foundation website.
Generally, when used as directed, over the counter analgesics are reasonably safe. On the other hand, long term or heavy use of drugs, especially those that contain a mixture of different painkilling medications in one capsule, have been associated with chronic kidney disease. Read the labels and beware should you see aspirin, acetaminophen and caffeine, for example, all in one pill.
Almost everyone will have head neck pain periodically.
Why? For many reasons, but not least that there are few of us who have not had a car accident, fallen down the stairs or taken a tumble from a horse or bicycle. Getting out of bed in the morning is dangerous but there's only one thing more dangerous; not arising from your slumbers.
Why? For many reasons, but not least that there are few of us who have not had a car accident, fallen down the stairs or taken a tumble from a horse or bicycle. Getting out of bed in the morning is dangerous but there's only one thing more dangerous; not arising from your slumbers.
Most people die in their beds.
Head Neck pain
But seriously, just when is the right time to go to your doctor or chiropractor, (sorry, got that wrong: your chiropractor, or your doctor) with neck pain and headaches? Yes, we really do know what causes headache.
Neck pain treatment
"How bad is my head neck pain?" is a question you may have been asking yourself. "Am I being a baby with a low pain threshold, or do I actually have a problem?"
A few thoughts. Just because you have a pain in the neck, or elsewhere, does not mean you must rush off to the chiropractor or your doctor. But then when should you go?
These are my golden tips. If you have
- Really severe pain,
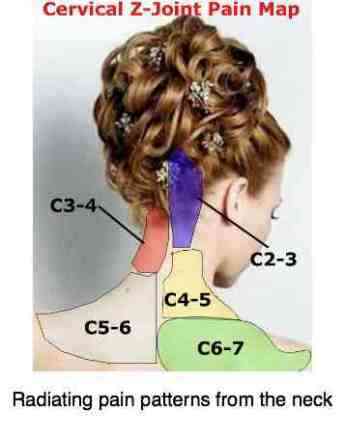
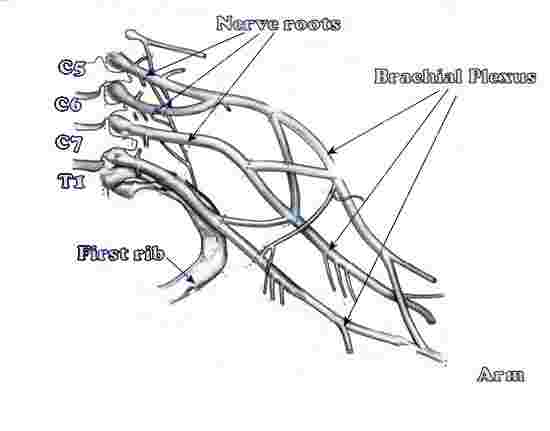
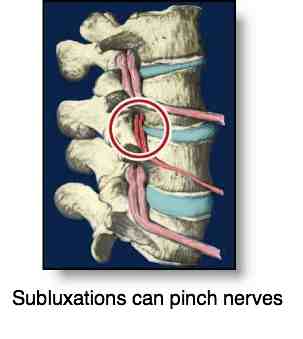
- Neck pain which radiates down the arm
- Stiff neck and headache
- Neck pain and a fever
- Headache and a fever
- Pain which you know is not getting better
Now it's time to get help. After, mm, how many days? That's difficult to say; it's best to use your own intuition. But recognise that if you arrive at the chiropractor with a pain you have had for three months or more, the definition of chronic, then you will certainly need more than a few treatments.
What's more, research shows that if you've had neck pain for over six months then, no matter what treatment you have, it's with you for life. It can be managed, helped, reduced, relieved, but it won't ever go away completely.
For an acute problem that has only begun in the last few days or weeks, as a rule, after a short course of chiropractic neck pain treatment, one may expect the problem to go away completely. Better still, if you go through a short course of rehabilitation, there's a good chance that it won't return for a long time.
But if you've had head neck pain for months or years, it is more difficult for your chiropractor to give you an assurance that your symptoms will recede completely. Don't wait too long. But don't go too soon either unless it's really severe, or you have a pinched nerve that radiates down your arm.
Then you really shouldn't wait; arm pain probably won't go away on its own.
If you're handy you can make a home traction unit that is very effective against head neck pain particularly if it radiates to the arm; make it yourself for a fraction of the cost of a commercial unit.
One of the great things about the chiropractic adjustment is that it's rarely painful. Artfully done, even with severe neck pain, and you're terrifiied that he or she is going to hurt you, or make it worse, it's rare that the cervical adjustment is painful.
Just this week, a lady with very severe neck pain; just one adjustment, no pain from the treatment, and she's eighty percent better; it's not always like that, especially if there's also arm pain.
Make sure you tell as accurately as possible any old injuries and illnesses that you may have had. I certainly, and I presume others have too, missed that a patient has had breast cancer, for example. It's not common but every chiropractor will have had patients who have metastases from an old, and presumed quiescent, cancer. That's why a complete lifestyle change is so important after cancer. Never accept the we got it all statement; don't live in terror of cancer but do change what you eat, and don't eat. Changing to a healthy lifestyle is important for us but particularly for the cancer patient. Otherwise it just comes back, often years later.
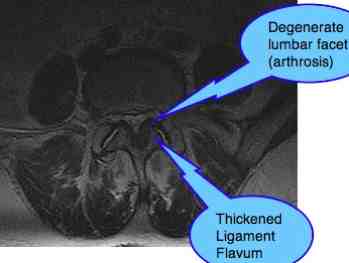
Or a car accident that happened thirty years ago, and was presumed irrelevant. It's those old injuries that cause the chronically fixated joints that become arthritic.
In the interim, a good massage from your spouse may relieve your head neck pain, particularly for back of head headaches, use some alternating ice and heat, do a few simple exercises, and don't go playing silly twits! This is not the time for a game of rugby, or lifting pianos. Avoid carrying heavy groceries on the affected side.
A strong recommendation ...
Research indicates that if you have neck pain for six months, then YOU WILL PROBABLY HAVE IT FOR THE REST OF YOUR LIFE. Once you know it's not going to get better of its own accord, then do something -- or spend the rest of your life suffering from head neck pain.
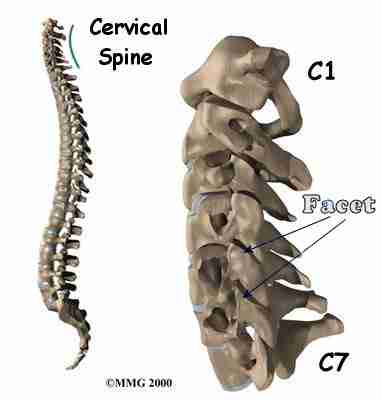
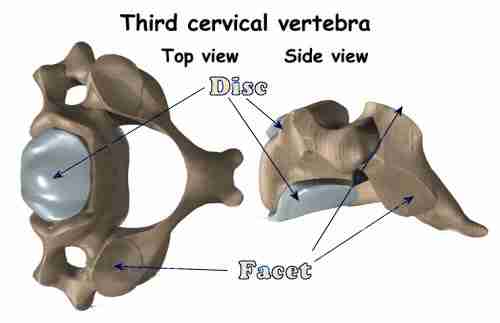
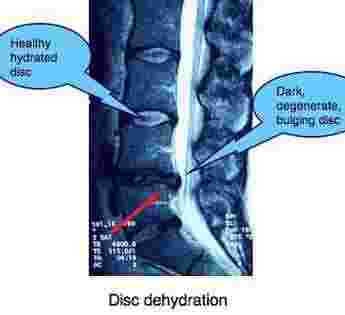
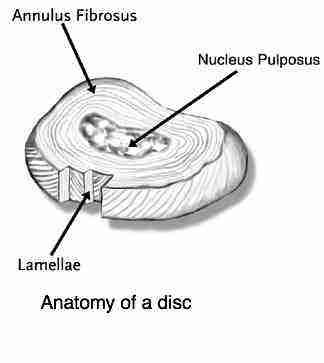
Why is that? Frankly, we're not totally certain but what we do know is that the hyaline cartilage in the little bones in your neck is very sensitive to subluxations - it's now proven that the cartilage begins to degenerate within 13 hours (in white mice anyway).
But if you've had head neck pain for months or years, it is more difficult for your chiropractor to give you an assurance that your symptoms will recede completely. Don't wait too long. But don't go too soon either unless it's really severe, or you have a pinched nerve that radiates down your arm.
Then you really shouldn't wait; arm pain probably won't go away on its own.
If you're handy you can make a home traction unit that is very effective against head neck pain particularly if it radiates to the arm; make it yourself for a fraction of the cost of a commercial unit.
One of the great things about the chiropractic adjustment is that it's rarely painful. Artfully done, even with severe neck pain, and you're terrifiied that he or she is going to hurt you, or make it worse, it's rare that the cervical adjustment is painful.
Just this week, a lady with very severe neck pain; just one adjustment, no pain from the treatment, and she's eighty percent better; it's not always like that, especially if there's also arm pain.
Make sure you tell as accurately as possible any old injuries and illnesses that you may have had. I certainly, and I presume others have too, missed that a patient has had breast cancer, for example. It's not common but every chiropractor will have had patients who have metastases from an old, and presumed quiescent, cancer. That's why a complete lifestyle change is so important after cancer. Never accept the we got it all statement; don't live in terror of cancer but do change what you eat, and don't eat. Changing to a healthy lifestyle is important for us but particularly for the cancer patient. Otherwise it just comes back, often years later.
Or a car accident that happened thirty years ago, and was presumed irrelevant. It's those old injuries that cause the chronically fixated joints that become arthritic.
In the interim, a good massage from your spouse may relieve your head neck pain, particularly for back of head headaches, use some alternating ice and heat, do a few simple exercises, and don't go playing silly twits! This is not the time for a game of rugby, or lifting pianos. Avoid carrying heavy groceries on the affected side.
A strong recommendation ...
Research indicates that if you have neck pain for six months, then YOU WILL PROBABLY HAVE IT FOR THE REST OF YOUR LIFE. Once you know it's not going to get better of its own accord, then do something -- or spend the rest of your life suffering from head neck pain.
Why is that? Frankly, we're not totally certain but what we do know is that the hyaline cartilage in the little bones in your neck is very sensitive to subluxations - it's now proven that the cartilage begins to degenerate within 13 hours (in white mice anyway).
A simple classification system for head neck pain
- Grade I head neck pain:
No signs or symptoms suggestive of major structural pathology (ie no severe pain, no radiation, no recent trauma) and no interference with activities of daily living. This will likely respond to those simple things suggested above; it does not usually require intensive investigations or ongoing treatment.
- Grade II cervical neck pain:
No severe pain or radiation, but now begins to interference with activities of daily living. You wake in the night with pain. You can't turn your head, and driving the car is thus dangerous. After a week or ten days, you have to acknowledge that it's not really improving. Then we suggest it's time to make an appointment with your chiropractor (or even your doctor first, if that is your first choice). A good examination is in order, and perhaps some early intervention aimed at preventing long-term disability.
- Grade III cervical neck pain:
with the onset of neurological symptoms. Headache, radiation pain or tingling down the arm, or into the midback. Now it's definitely time to get help, particularly if it has lasted for more than a few days.
- Grade IV cervical neck pain:
Still no signs or symptoms of major structural pathology, but presence of neurologic signs such as decreased deep tendon reflexes, weakness, and/or sensory deficits. In my opinion it is now definitely time for x-rays, perhaps even a scan. The pain of a pinched nerve in neck is often severe, the ache in your arm something you cannot escape, no matter how you change your position. It's often worst at night. This head neck pain should no longer be ignored.
- Grade V neck pain: Signs or symptoms of major structural pathology, such as fracture, myelopathy, neoplasm, or systemic disease; requires prompt investigation and treatment, and probably a consultation with a specialist. Certainly if the condition is not responding within a few weeks to conservative treatment.
- Grade I head neck pain:
- No signs or symptoms suggestive of major structural pathology (ie no severe pain, no radiation, no recent trauma) and no interference with activities of daily living. This will likely respond to those simple things suggested above; it does not usually require intensive investigations or ongoing treatment.
- Grade II cervical neck pain: No severe pain or radiation, but now begins to interference with activities of daily living. You wake in the night with pain. You can't turn your head, and driving the car is thus dangerous. After a week or ten days, you have to acknowledge that it's not really improving. Then we suggest it's time to make an appointment with your chiropractor (or even your doctor first, if that is your first choice). A good examination is in order, and perhaps some early intervention aimed at preventing long-term disability.
- Grade III cervical neck pain: with the onset of neurological symptoms. Headache, radiation pain or tingling down the arm, or into the midback. Now it's definitely time to get help, particularly if it has lasted for more than a few days.
- Grade IV cervical neck pain: Still no signs or symptoms of major structural pathology, but presence of neurologic signs such as decreased deep tendon reflexes, weakness, and/or sensory deficits. In my opinion it is now definitely time for x-rays, perhaps even a scan. The pain of a pinched nerve in neck is often severe, the ache in your arm something you cannot escape, no matter how you change your position. It's often worst at night. This head neck pain should no longer be ignored.
- Grade V neck pain: Signs or symptoms of major structural pathology, such as fracture, myelopathy, neoplasm, or systemic disease; requires prompt investigation and treatment, and probably a consultation with a specialist. Certainly if the condition is not responding within a few weeks to conservative treatment.