Knee Strengthening Exercises
Knee strengthening exercises are one of the best ways to cure knee pain. People who do them have less pain, recover quicker from injuries, function better and have less chance of problems recurring in the future.
Knee strengthening exercises can be used to help relieve and sometimes even prevent various causes of knee pain. Whenever there is weakness in the leg muscles, it means the knee joint is less well supported, resulting in more weight going through the bones, therefore making knee problems much more likely.
Where To Start
There are so many different knee strengthening exercises out there, it can be hard to know where to start. Here I share with you my favourite exercises grouped by muscle – easy to perform, quick, effective and suitable for most people.
1) Quads Strengthening: Front thigh muscles that straighten the knee
2) Hamstring Strengthening: Back thigh muscles that bend the leg
3) Glutes Strengthening: Buttock muscles play a crucial role in controlling then knee
4) Calf Strengthening: Lower leg muscles that control the foot
5) Combination Strengthening: Strengthen all the muscle groups at once
6) Balance Training: How to improve your balance
2) Hamstring Strengthening: Back thigh muscles that bend the leg
3) Glutes Strengthening: Buttock muscles play a crucial role in controlling then knee
4) Calf Strengthening: Lower leg muscles that control the foot
5) Combination Strengthening: Strengthen all the muscle groups at once
6) Balance Training: How to improve your balance
Pick and choose the ones you find challenging but not painful. If they are too easy for you, visit the Intermediate and Advanced knee strengthening exercise sections.
To find out how to exercise safely and effectively, visit the sections on How to Exercise Right and Getting the Best Results from your knee strengthening exercises.
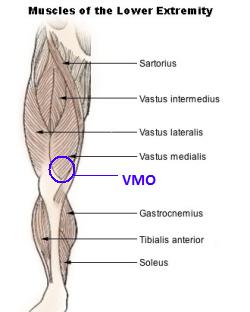
Quads Knee Strengthening Exercises
These are the muscles at the front of the thigh that straighten the knee. Weak quads is one of the most common causes of pain making quads knee strengthening exercises an important part of any rehab programme.
1) Quad Clenches
Purpose: Maintain and strengthen the Quads without moving the knee, enable full straightening of the knee
Starting position: Lying flat on your back or sitting up. Leg and knee straight
Action: Tighten the muscle on the front of the thigh by pushing your knee down. You should feel your thigh muscles clench. Hold for 3 secs
Repetition: Repeat 10-20x every 3-4 hours
Variations: If you are struggling to get your knee to straighten fully, place a rolled up towel underneath the ankle so that your leg is lifted slightly on the bed. Then do the exercise as described. Lifting the knee up slightly lets gravity help the knee to straighten
2) Short Arcs
Purpose: Strengthen the quads muscles without much knee movement

Starting position: Lying flat on your back or sitting up with your leg horizontal on a flat surface such as a bed. Place a rolled up towel (approx 10cm diameter) under the knee.
Action: Pull your toes towards you and clench you thigh muscles. Slowly lift your foot up off the bed until your knee is straight (keep your knee resting on the towel). Hold for 3-5 secs and slowly lower
Repetition: repeat 10-20 times, 3x daily
Progression: 1) Increase the size of the towel under the knee 2) Add a weight e.g. by wearing a shoe, or using a light ankle weight. Progress further by using a heavier weight
3) Straight Leg Raise
Purpose: Strengthen the Quads muscles without bending the knee NB Do not do this if you have a history of back problems
Starting position: Lying flat on your back. Leg and knee to be worked straight, other leg bent
Action: Pull your toes towards you and tighten/clench the muscle on the front of the thigh, locking your knee straight. Lift your foot up about 6 inches off the bed. Hold for 3-5 secs and slowly lower. Ensure your knee stays straight the whole time
Repetition: repeat 10-20 times, 2x daily
Progression: 1) Add a weight e.g. by wearing a shoe
4) Long Arcs
Purpose: Strengthen quads, increase knee mobility, great to do anytime sitting for prolonged periods (30mins+) to stop the knee getting stiff -
Starting position: Sitting on a firm chair with your knee bent and your foot on the floor
Action: Lift your foot up and straighten your knee as much as possible. Hold for 3-5 secs and slowly lower
Repetition: 5-20 times, 3xdaily
Progression: Strengthen further by adding an ankle weight
5) Knee Marching
Purpose: Increase quads strength without putting weight through the knee join
Starting Position: Sit in a chair with your feet on the floor
Action: March your legs up and down one at a time. Lift your knee and foot up and then back down
Repetition: Repeat for about 1 minute, 2x daily and any time you are sitting for more than 20 minutes to stop your knee getting stiff
Progression: Add a weight
Hamstring Strengthening Exercises
The hamstrings are the muscles on the back of the thigh that bend the knee. You need a good combination of strength and length in the muscles. These hamstring knee strengthening exercises are a great place to start.
1) Hamstrings Clenches
Purpose: Strengthen the hamstrings muscles without having to move the knee
Starting Position: Sit in a chair with your heel against the leg of the chair and your feet firmly on the floor
Action: Press your heel firmly backwards into the chair leg feeling the back of your thigh tightening/clenching. Hold for 3-5 secs
Repetition: Do 10-20x, 2x daily
Note: The foot shouldn’t move during this exercise
2) Buttock Kicks
Purpose: Strengthen hamstrings without any weight going through the knee joint, increase knee mobility (flexion), aid circulation
Starting position: Lie on your tummy (on the floor or bed) with your legs straight
Action: Lift your foot off the floor and bring it towards your bottom as far as you can. Slowly return to the starting position
Repetition: Repeat 10-25x, 3x daily
Notes: 1) You are aiming to get your heel all the way to your bottom 2) Make the exercise easier by hooking your good leg underneath the bad and using it to help lift the bad leg up
Progression: Add a weight e.g. a shoe or ankle weight
3) Kick Backs
Purpose: Improve the strength of hamstrings and mobility of the knee
Starting Position: Stand up straight holding on to something stable e.g. chair or table
Action: Lift your foot up as far as you can towards your bottom, bending the knee. Hold for 3-5 secs
Repetition: Do 5-25 times, 2x daily
Progression: Add a weight e.g. shoe or ankle weight
Note: 1) Don’t bend forwards - keep your body upright 2) keep your knees in line with each other- don’t let your thigh come forwards
4) The Bridge: Stage 1
Purpose: Excellent knee strengthening exercises for the hamstrings,
Starting Position: Lie on your back with both knees bent about 90° and your feet on the floor/bed
Action: Clench your buttocks and lift your bottom off the bed as high as you can without arching your back. Hold for 3-5 seconds and slowly lower
Repetitions: Repeat 10-25 times, 1-2x daily
Note: 1) Keep your back straight – don’t let it arch as you lift up, it should be your bottom doing the work 2) Don’t hold your breath – keep breathing normally
Glutes Knee Strengthening Exercises
These are the buttock muscles, vital for ensuring the forces go through the knee evenly. The glutes are often forgotten about in knee strengthening exercises. Virtually everyone who suffers from knee pain has weak glutes, so they are well worth doing.
1) Buttock Clenches
Purpose: Maintain and strengthen the Glutes without the knee moving
Starting position: Lying down or sitting up.
Action: Clench your buttocks together and hold for 3 seconds. You should feel yourself rise up slightly
Repetition: Repeat 10-20x every 3-4 hours
2) The Clam
Purpose: Strengthen the glutes to help support the knee and prevent excessive weight going through the inner side of the knee – a must for anyone with knee pain!
Starting position: Lie on your side with your hip and knees bent approx 90°, feet together.
Action: Keeping your feet together, lift the top knee up as high as you can. Hold for 3 seconds and slowly lower
Repetition: Repeat 10-25x on each side, 2x daily
Note: Do not let your top hip roll backwards
Calf Strengthening Exercises
The calf muscles can be found on the back of the leg between the knee and the ankle. The move the foot and ankle, and help support the knee so should always been included with knee strengthening exercises.
1) Heel Raises
Purpose: Strengthen the calf muscles to help support the knee
Starting position: Stand with your feet slightly apart, weight equally distributed, holding onto something solid for balance
Action: Rise up onto your toes lifting your heels as high as possible. Keep your body upright (don’t bend forwards). Hold for 3-5 secs and slowly lower
Repetition: Repeat 10-30 times, 2x daily
Combination Knee
Strengthening Exercises
Here you will find knee strengthening exercises that work two or three muscle groups at the same time.
1) Sit to Stand
Purpose: improve knee mobility, strengthen quads and glutes, improve general fitness
Starting position: Sit in a firm chair, feet on the floor
Action: Lean forwards, lift your bottom and stand up straight and then sit back down
Repetition: Repeat 10-30x
Notes: 1) You can make this exercise easier by pushing up through your arms too 2) The higher the chair, the easier the exercise
Progression: 1) Don’t use your arms 2) Use a lower chair 3) Increase the speed you do the exercise at 4) Hold a heavy weight – e.g. bag of books during the exercise
Balance / proprioception is really important to prevent knee injuries, and is often reduced with knee arthritis. As a quick test to see whether you would benefit from balance knee strengthening exercises try standing on one leg with your eyes closed. If you can’t do it for one minute, you would benefit from this exercise. This exercise helps your body learn the subtle adjustments needed for good balance.
1) One Leg Standing: Stage 1
Starting position: Standing near a wall or chair for support
Action: Lift up your good leg and stand on one leg for as long as you can. It is normal to wobble a bit
Repetition: Spend 5 minutes doing this 2x daily e.g. when brushing your teeth
Progression: 1) Close your eyes and perform the exercise as above - you'll be surprised how much harder it is
What Next?
As your muscles get stronger, you will be able to increase the number of repetitions of each of these knee strengthening exercises.
You will probably need to do knee strengthening exercises at least four times a week for about a month before you notice much change in your knee pain.
When you feel ready, strengthen your muscles further by progressing on the intermediate and advanced knee strengthening exercises.
- See more at: http://www.knee-pain-explained.com/knee-strengthening-exercises.html#sthash.hxrnffJL.dpuf




.jpg)
.jpg)
.jpg)
.jpg)